Many people don’t realize the effects of preeclampsia last way beyond the initial pregnancy or postpartum period. I didn’t realize it myself until I started sharing my birth story with preeclampsia online and discovered the Preeclampsia Foundation several months postpartum. These effects often don’t show up until much later in a survivor’s life. This can make it scary to experience because many survivors were in good health before developing preeclampsia.
Disclaimer: Knock on Motherhood is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com.
note: in this blog post. The term "preeclampsia" will be an umbrella term for HELLP Syndrome and eclampsia. Both in pregnancy and postpartum
Table of Contents
Are there long-term effects of preeclampsia?
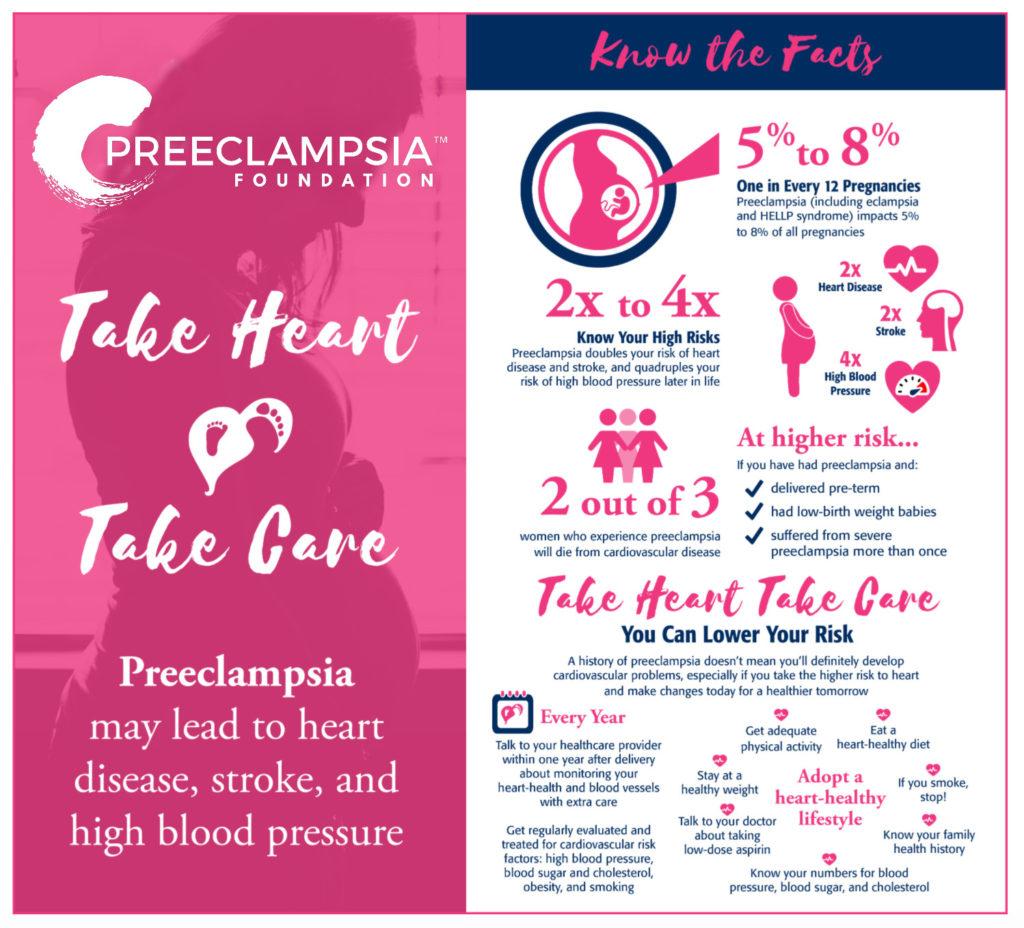
There are long-term effects of preeclampsia on the mother. Women who develop preeclampsia during their pregnancy or postpartum period have 3-4x times the risk of developing high blood pressure and 2x times to develop heart disease later in life. Preeclampsia survivors also have a higher risk to develop diabetes. Those preeclampsia survivors are at a higher risk if they gave birth prematurely, had babies that were low birth weight, and had severe preeclampsia more than once. According to the Preeclampsia Foundation, it is still unknown if this risk is due to preeclampsia or if these women were already predisposed.
- 3-4x Risk to Develop High Blood Pressure
2. 2x Risk to Develop Heart Disease
3. 2 out of 3 women who develop preeclampsia will die from cardiovascular disease
4. 2x risk to develop a stroke
5. Higher risk if you delivered preterm, had low-birth weight babies or suffered from preeclampsia more than once
The Preeclampsia Foundation’s position paper titled, “Preeclampsia and Future Cardiovascular Disease in Women: What Do We Know and What Can We Do”, says, “Women with preeclampsia have been noted to have CVD [cardiovascular disease] and thromboembolic events as early as 5 to 10 years following the index pregnancy.”
In that same paper, it is noted that there are 2 possible theories of why women who had preeclampsia have a higher risk for cardiovascular disease.
2 Possible Theories of Why Preeclampsia Survivors Have a High Risk for Cardiovascular Disease
- Preeclampsia causes long-term damage to the body, especially the heart and blood
vessels. This damage could put women at high risk for cardiovascular disease later in life. - A woman who gets preeclampsia already had a less healthy heart and blood vessels.
Then, when she becomes pregnant, her pregnancy stresses her blood vessels and heart even more and results in preeclampsia.
These risk factors can be scary to learn, but just because there is a risk factor doesn’t mean it is a guarantee a preeclampsia survivor will develop it. As I always say when sharing research about preeclampsia, knowledge is power. Because we have the knowledge of the risk factors of developing heart disease, stroke, diabetes, and chronic high blood pressure, we can make the necessary lifestyle changes to lower our risk as much as we can.
Risk factors Preeclampsia Survivors Can Reduce:
- Reduce weight to no longer be overweight or obese
- Lower High Blood Pressure (greater than 140/90)
- Lower High Blood Sugar
- Lower High Blood Triglycerides
- Stop Smoking

What Can I do as a preeclampsia survivor to help my long-term health?
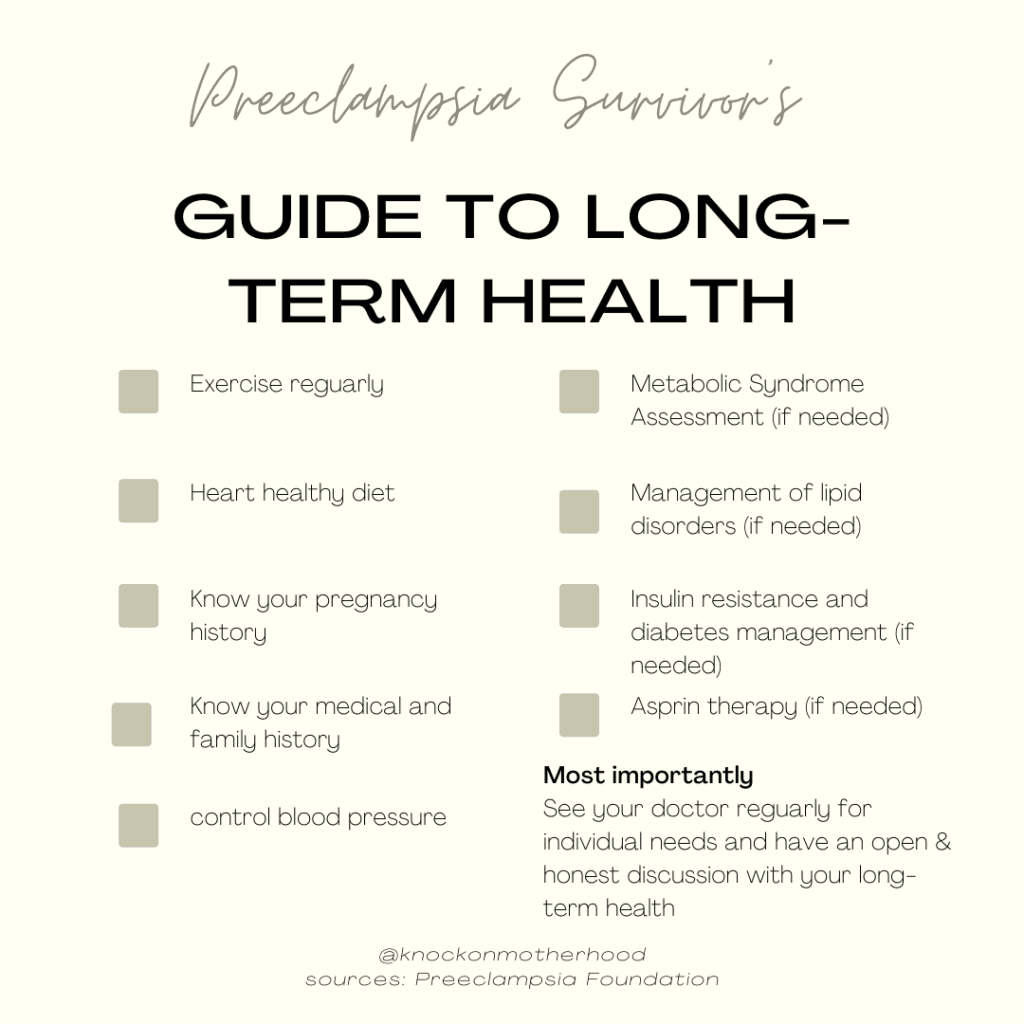
- Exercise regularly
Preeclampsia survivors should focus on an exercise routine that is sustainable to maintain lifelong health. Aim for 30 minutes 5 times a week of a cardio-type movement such as a walk, YouTube video, or jog. 2-3 times a week do some sort of strength exercise to build or maintain muscle to help you be able to keep doing all the activities you want to be able to do throughout your life.
2. Eat a heart-healthy diet
The DASH (Dietary Approaches to Stop Hypertension) has been proven to lower blood pressure. (Mayo Clinic). Even if you don’t have high blood pressure, eating this way can help you create heart-healthy habits and prevent or delay future cardiovascular problems.
According to the Preeclampsia Foundation, “Evidence on effective interventions for these women is limited. Berks etal. used statistical modeling to estimate the effects of lifestyle modifications, such as regular exercise and a healthy diet, on the risk of CVD in women with a history of preeclampsia and found that such interventions could decrease the risk by between 4% and 13%.
3. Know your pregnancy history
Both you and your doctors should know your pregnancy history. Women who had preeclampsia with a preterm delivery (>37 weeks) or recurrent preeclampsia especially have an increased risk. These women should have an annual assessment of their blood pressure, lipids, fasting glucose, and BMI to check on their health.
Don’t know what to chat with your doctor about? Read my post titled: After Preeclampsia: 30 Amazing Questions to Ask Your Doctor
4. Know your medical and family history
The ACC and AHA guidelines for the assessment of CVD risk recommend that all men and
women ages 20 to 79 be screened for traditional risk factors every four to six years. Preeclampsia survivors should look into their family history for the history of preeclampsia, early cardiovascular disease or other cardiovascular events (such as blood clots, strokes, etc), and diabetes. Family history combined with personal history can help identify early signs and risk factors.
5. Control blood pressure
Preeclampsia survivors need to have conversations with their doctors on how to control their blood pressure, especially for those who have chronic high blood pressure. The use of medications can be helpful as well as lifestyle changes. It is also important to have a home blood pressure cuff to know your numbers and what is normal for you.
6. Metabolic Syndrome Assessment
Preeclampsia survivors need to be assessed for obesity, hypertension, dyslipidemia, and abnormal glucose metabolism. There should be a glucose screening annually.
7. Management of lipid disorders
According to the Preeclampsia Foundation, “Disorders of lipid metabolism often occur in conjunction with hypertension as well as impaired insulin sensitivity. A fasting lipid panel should be checked periodically in preeclampsia survivors due to an increased incidence of abnormal cholesterol levels in this population.”
8. Insulin resistance and diabetes
Preeclampsia survivors have a higher incidence of insulin resistance. “It may be reasonable to screen patients with a history of preeclampsia for diabetes or impaired fasting glucose” (Preeclampsia Foundation).
9. Aspirin Therapy
In the case of preeclampsia survivors, aspirin is typically given during the next pregnancy before 16 weeks gestation. “The USPSTF and ACOG now both recommend low-dose aspirin for the prevention of preeclampsia” (Preeclampsia Foundation).
10. See your doctor regularly
It is so important to have a great relationship with your doctor after preeclampsia. As a preeclampsia survivor, your doctor can help guide you in the right direction to improve your health or prevent future problems. A common question survivors ask is “Should I see a cardiologist after preeclampsia?” That is a question that is individualized to each survivor, but in my non-medical advice, it would never hurt to ask your doctor if seeing a cardiologist will be right for you.
How I Take Care of My Health Long-Term as a Preeclampsia Survivor
I try and be transparent with how preeclampsia has affected my health long term over on my Instagram. I think it is important to do it so other preeclampsia survivors know they aren’t alone in their struggles.
High Blood Pressure
I was on high blood pressure medication until I was 8 weeks postpartum. I have been fortunate to not need them since. My blood pressure has stayed within normal range and I haven’t had any sort of problem since. I use this blood pressure cuff to keep up to date with my blood pressure readings. I am currently pregnant so I take it every day, but when I am not pregnant I do it a few times a month.
Insulin Resistance
When I was a little over a year postpartum I went to go see my new primary care doctor. I had moved cities, so I had a different doctor. I originally went to see him for a general annual checkup and brought up concerns about being exhausted no matter how long I slept and my inability to lose weight. I was so tired that I would sleep during every single nap that my baby took as well as sleep at night. I was frustrated with the lack of weight loss because I felt I was doing what I needed to do to be able to see the results I wanted.
At that appointment, I was prescribed an antidepressant/anti-anxiety medication to see if that would help my exhaustion and depression. A month or so later at a follow-up, I was prescribed Metformin because my blood work showed a slight insulin resistance, making it more difficult for me to be able to lose weight.
UPDATE AS OF 2023: I got off metformin a little over a year after being prescribed. I hated the side effects. I also have not had an issue since. It seems my body just needed some extra help and time to heal.
Hypothyroidism
About 2 years postpartum, I met with my primary care doctor again. I didn’t like the side effects that Metformin gave me and wanted to get off of it. I was able to get off. I had also weaned off the antidepressant/anti-anxiety medication at this point. I was still experiencing exhaustion and hair loss. My primary care doctor ran some blood work and determined I had hypothyroidism and got me on a medication called Levothyroxine. Ever since I got on that medication I have felt so much better. No longer exhausted and I have been able to see the progress in weight loss I wanted to see to get in a healthier place for me.
UPDATE AS OF 2023: I have been on levothyroxine for almost 2 years and have continued on it during my current pregnancy. My OBGYN has been running labs every so often to check my levels to make sure they stay stable.
Blood Clot
About 2.5 years postpartum I got a blood clot in my leg. It was very painful and swollen. I was fortunate enough to have caught it early and have mostly been able to take care of it with at-home care along with visits to my hematologist. I was on blood thinners for a few months to help break up the clot, but have been able to get off of them. I now need to wear compression socks and elevate my leg at the end of the day. I still have a slight clot, but I have been able to manage it mostly at home through the guidance of my hematologist.
I’m not sure if all of these health problems occurred because of preeclampsia or if I already had a predisposition for them. I have a strong family history of blood clots and have been tested for all of the different disorders. I did not test positive for any of them, however, my hematologist suspects there is something that science hasn’t found yet because of the family history of blood clots. Either way, according to the latest research I shared above having preeclampsia did increase my risk for insulin resistance and blood clots.
Preeclampsia Survivors Don’t Need to be Scared About These Statistics
It can be overwhelming to implement every single recommendation into your life, especially if you are a recent preeclampsia survivor. Remember that any little thing you can do can help your future health. Take things in baby steps. For instance, if you do not have a regular exercise routine it can be hard to immediately do 5 days a week. Try to take a walk once a week and then work your way up to 5 or more. This same approach can be used with eating healthy as well. If you aren’t used to eating fruits and veggies, just adding one portion a day and slowly adding more to your diet will make the transition easier.
I am not sharing all this information to scare you. As I mentioned earlier, knowledge is power, especially for preeclampsia survivors. We don’t know a lot about preeclampsia but we do know that preeclampsia survivors have a high chance to develop diabetes or cardiovascular problems and there are tools we can use to help prevent it.
Can you have a healthy pregnancy after preeclampsia?
Absolutely. Although preeclampsia survivors have a higher risk to develop preeclampsia in a second pregnancy, it is not a guarantee. Low-dose aspirin is typically given before 16 weeks gestation in the next pregnancy after preeclampsia and it is one of the only things that will help prevent preeclampsia (ACOG).
UPDATE AS OF 2023: I am pregnant again after preeclampsia and have shared my journey over on this post.
Can I have another baby if I had preeclampsia?
In a lot of cases, it is physically possible to have another baby after preeclampsia. Many women decide to expand their family through pregnancy after preeclampsia but there are also some who do not. This answer is completely up to the preeclampsia survivor on what they want to do. Preeclampsia survivors need to have an honest and open conversation with their OBYGN and MFM on the risk factors they have and how the next pregnancy will go.
In summary, there are risks that occur after surviving preeclampsia. There are so many factors we are able to control to help us minimize the risk of developing conditions such as chronic high blood pressure, cardiovascular disease, and diabetes. I wish there was more research on preeclampsia to help not only me but other preeclampsia survivors with their future health. I hope one day there is. For now, we know the few things we can control and we need to let that be our guide. Knowledge is power.
If you would like to stay up to date with me, join my community on Instagram, Facebook, Pinterest, and subscribing to my email list.
Did you know I co-host the Knock on Parenthood Podcast?
You May Like: